Research
Nanotechnology
 Cancer Biology
Cancer Biology
BESTeam focuses on the development and use of innovative magnetic resonance imaging and
fluorescence intravital cell tracking methods for cancer applications. MRI provides
noninvasive 3D whole animal imaging to allow for early cancer detection strategies,
follow tumor growth dynamics and track the distribution of magnetically labeled
cells, whereas, live fluorescence imaging of the murine tumor vasculature provides
information on tumor and blood cell morphology, adhesive interactions and migration
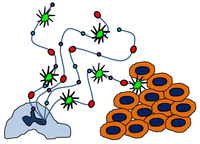
patterns within <1 second. We have three main research areas of emphasis: 1)
development of new targeted MRI nanoparticle contrast agents for early cancer detection,
2) use of
in vivo fluorescence confocal microscopy to elucidate the role of the tumor
microenvironment, specifically neutrophils and platelets, in promoting metastasis
and 3) inhibition of metastasis through creation of targeted drug delivery approaches.
Currently, we have two on-going projects:
pH-sensitive manganese oxide particles for early cancer detection
A common characteristic of tumors is an acidic extracellular pH of 6.5–6.9. Lactic acid builds up in the tumor extracellular space due to high tumor cell metabolism of glucose to form ATP. Previously, we have introduced manganese oxide poly(lactic-co-glycolic acid) nano- and micro-particles as pH-sensitive smart MRI contrast agents for labeling tumor cells (Bennewitz et al., ACS Nano, 2011). At low pH, MnO cores dissociate into Mn2+ and the free Mn2+ interacts with surrounding water molecules to cause positive contrast on T1 MRI. At physiological pH 7.4, MnO does not dissolve to form Mn2+ and therefore, minimal contrast is generated on MRI in the absence of a drop in pH. Within a tumor, MnO PLGA nanoparticles can create positive MRI contrast through dissolution in the acidic extracellular space (~pH 6.5) or upon cellular endocytosis and subsequent shuttling to low pH endosomes and lysosomes (~pH 5) within cancer cells.
Electron microscopy of A) MnO cores, B) MnO PLGA nanoparticles and C) MnO PLGA microparticles. A) Transmission electron microscopy showed 15-20 nm aggregates of several 5-10 nm cores. B, C) Scanning electron microscopy of nano- and micro-particles showed that particles had a smooth spherical morphology. Nano- and micro-particle size was approximately 140 nm ± 50 nm and 1.7 ± 0.9 μm, respectively. MnO cores were dispersed throughout the PLGA particles as shown by TEM images (insets). Figure adapted from Bennewitz et al., ACS Nano, 2011.
Controlled release of A) MnO PLGA nanoparticles (NPs) and B) MnO PLGA microparticles (MPs) in PBS pH 7.4 (dashed lines) and 20 mM citrate pH 5 (solid lines). Note significant release of Mn2+ from particles incubated in citrate pH 5 but not PBS pH 7.4. Figure from Bennewitz et al., ACS Nano, 2011.
Role of tumor microenvironment in promoting metastasis
Previously, we developed a multiphoton imaging technique called quantitative
fluorescence intravital lung microscopy with a vacuum stabilized window
to track the migration of blood cells in the pulmonary microcirculation of live
sickle cell disease mice (Bennewitz et al.,
IntraVital, 2014). Using qFILM, we discovered that neutrophils and
platelets formed large aggregates in sickle cell disease mice given a small dose
of an inflammatory stimulus; these aggregates were unable to pass through the
“arteriolar bottlenecks” located at the junction of pulmonary arterioles and
capillaries (Bennewitz et al.,
JCI Insight, 2017). Similar to sickle cell disease, cancer is also
an inflammatory condition in which neutrophils and platelets are activated. Through
utilizing qFILM, we are investigating the role of neutrophils and platelets in
promoting metastasis. The cross-talk between neutrophils, platelets and cancer
cells remains to be fully elucidated. Previous studies have shown that activated
platelets can bind to neutrophils to facilitate the release of neutrophil extracellular
traps including neutrophil DNA, histones and granular content. Tumor cells
can also directly activate neutrophils to cause NET release through secretion
of soluble factors. NETs can trap circulating tumor cells and further activate
platelets to cause thrombosis. Other stimuli for NET release remain to be discovered.
There has also been evidence of NETs within cancer patient samples, providing
clinical relevance.
Schematic of qFILM setup. A catheter is placed into the carotid artery to enable delivery of intravascular fluorochromes and fluorescent antibodies. The mouse is intubated to facilitate mechanical ventilation and delivery of 1% isoflurane with FiO 2 of 0.95. The temperature of the mouse is maintained with a heated stage. Gentle vacuum suction is applied to the thoracic window device to immobilize a small region of the left lobe of the lung against a cover glass. Physiological monitoring can be achieved through blood pressure measurement using the carotid artery catheter and by pulse oximetry. Figure from Bennewitz et al., IntraVital, 2014.
qFILM reveals large neutrophil-platelet aggregates in pulmonary arterioles in sickle cell disease mice. A) Four large aggregates of neutrophils (red) and platelets (green), marked by dotted circles, are shown blocking pulmonary arteriolar bottlenecks in a sickle cell disease mouse. The pulmonary microcirculation is shown in purple. Red arrows indicate aggregates with mostly neutrophils bound to a small number of platelets and green arrows indicate aggregates with mostly platelets bound to a small number of neutrophils. B) Larger view of a neutrophil predominant aggregate from A). C) Larger view of a platelet predominant aggregate from A). Figure adapted from Bennewitz et al., JCI Insight, 2017.
Movies in sickle cell disease mice using qFILM published in Bennewitz et al., JCI Insight, 2017:
neutrophil-platelet aggregates in a pulmonary arteriole in a sickle cell disease mouse
Pulmonary vaso-occlusions (white circles) blocking all 4 arteriolar bottle-necks in an SCD mouse administered 0.1 µg/kg IV LPS. Neutrophil vaso-occlusions (red arrows). Platelet vaso-occlusions (green arrows). White arrow-direction of blood flow. Pulmonary microcirculation (purple). 2/3x original acquisition rate.
embolic neutrophil-platelet aggregate formation leads to pulmonary vaso-occlusion
Embolic neutrophil-platelet aggregate occluding an arteriole in an SCD mouse administered 0.1 µg/kg IV LPS. A large aggregate of several neutrophils (red) with a few platelets (green) travels down the feeding arteriole and occludes the arteriolar bottle-neck. Pulmonary microcirculation (purple). 2/3x original acquisition rate.
in situ neutrophil-platelet aggregate formation leads to pulmonary vaso-occlusion
In situ nucleation of a neutrophil-platelet aggregate in the pulmonary arteriolar bottle-neck in an SCD mouse administered 0.1 µg/kg IV LPS. An aggregate (white circle) of three neutrophils (red) attached to a few platelets (green) slowly grows over time to an aggregate of five neutrophils which completely blocks an arteriolar branch. Pulmonary microcirculation (purple). 2/3x original acquisition rate.
lack of neutrophil-platelet aggregates following p-selectin inhibition
Neutrophils (red) and platelets (green) trafficking through the pulmonary microcirculation (purple) in an SCD mouse after 0.1 µg/kg IV LPS + anti-P-selectin mAb Fab fragments. A freely circulating neutrophil is seen trafficking up the arteriole into the capillaries. Pulmonary vaso-occlusion is absent. 2/3x original acquisition rate.